Medical treatment of the complication of first trimester pregnancy loss with misoprostol


Опубликована Сен. 30, 2014
Последнее обновление статьи Авг. 19, 2022
Abstract
The objective of the study was to evaluate the efficacy of misoprostol in patients with complication of first trimester pregnancy loss. After the departmental approval, a total of 102 women with first trimester pregnancy failure were recruited for treatment with misoprostol. The inclusion criteria were gestational age of less than 12 weeks and hemodynamically stable. The exclusion criteria were patients with history of hypersensitivity to prostaglandin, bronchial asthma and hemoglobin less than 9 g. Main outcome measures were the successful resolution of miscarriages without surgical intervention; secondary outcomes were incidence of pain, vaginal bleeding, infection, pyrexia and gastrointestinal side effects. A total of 102 women were included in the study. Age ranged from 16 to 40 years and parity ranged from 0 to grand multipara. Women were not selected according to parity but parity was a random occurrence. No relationship was found between parity and response to treatment with misoprostol. Incomplete abortion was found in 82 (80.39%), an embryonic pregnancy in 7 (6.86%) and early fetal demise in 13 (12.74%). 62.74% women completely expelled the conceptual products on treatment with misoprostol alone, while 38 (37.25%) patients required surgical evacuation due to incomplete expulsion of conceptual products. Mean induction to expulsion interval was 15.66 h. Main side effects noted were pain, pyrexia, nausea, vomiting and diarrhea. More than one side effect was noted in 7 (22.54%) patients. Treatment of early pregnancy loss with misoprostol is efficient, acceptable and cost effective for patients with complications of first trimester pregnancy loss.
Ключевые слова
Medical treatment, miscarriage., Misoprostol
INTRODUCTION
Post abortion care refers to the services required by women who have problems after pregnancy failure. Treatment is recommended in first trimester pregnancy loss to reduce morbidity like pelvic inflammatory disease (PID), hemorrhage, blood coagulation defects, and chronic pelvic pain in fertility. Medically, pregnancy loss is usually described as “incomplete” or “missed” abortion. An “incomplete abortion” is usually diagnosed when the woman has an open cervix and has passed some, but not all the products of conception. A “missed abortion” is diagnosed when a woman has a closed cervix, a uterus which does not increase in size and a non-viable embryo or fetus (an embryonic pregnancy or an embryonic/fetal demise). Terminology is embryo (0 to 8 weeks) and fetus (9 to 12 weeks).
There are different treatment options available for treat-ment of early pregnancy loss; the choice lies between expectant, surgical and medical treatment (Khan et al., 2007; Alberman, 1992; Macrow and Elstein, 1993). Expectant management is to wait for spontaneous abortion, but the success rate with the use of this approach for embryonic or fetal death or anembryonic gestation is suboptimal (ranging from 25 to 76%). The interval to spontaneous expulsion is unpredictable, and it may take a month. The uncertainty and anxiety, along with the sadness resulting from pregnancy loss, often make expectant management less appealing to patients (Ballagh et al., 1998; Jurkovic et al., 1998).
Surgical evacuation was the treatment of choice before medical treatment was used, but due to increased morbidity associated with surgical procedure, studies are ongoing to determine the efficacy and safety of medical treatment (Khan et al., 2007). Prostaglandins have emerged as the agents of choice for medical treatment of first trimester pregnancy loss.
Several studies have shown that medical treatment is a safe, effective and acceptable alternative to suction curet-tage. Misoprostol (15 deoxy-16 hydroxy 16 methyl PGE1) is a stable, synthetic form of prostaglandin E1 analogue. It was originally developed in 1970’s for the prevention of non-steroidal anti-inflammatory drugs (NSAID) induced peptic ulcers (Luise et al., 2002; Mazhar et al., 2013; Awan et al., 2008). Several clinical trials have evaluated the use of misoprostol alone for termination of early pregnancy failure (Bogratee et al., 2014; Beucher et al., 2003).
In the last two decades, medical termination of pregnancy has become a safe alternative to vacuum aspiration and dilatation and curettage (Blanchard et al., 2005; Borgatta et al., 2004; Creinin and Damry, 1993). The cost savings to the patient and family is extremely important, even if the misoprostol administration did not lead to uterine evacuation. It would soften the cervix and make surgical evacuation an easier procedure.
The objective was to study the efficacy of misoprostol in women with complication of first trimester pregnancy loss as this is cost effective for low resource population. Misoprostol has long been used in our country, but there are few studies regarding its use as abortificient.
METHODOLOGY
After the departmental approval, a total of 102 women with first trimester pregnancy failure were recruited for treatment with misoprostol. The women were given detailed information regarding different treatment options available, only women who accepted the medical treatment with misoprostol were selected. The inclusion criteria were gestational age of less than 12 weeks and hemodynamically stable. The exclusion criteria were patients with history of hypersensitivity to prostaglandin, bronchial asthma and hemoglobin less than 9 g. Gestational age was determined by clinical examination and ultrasound.
All women were given detailed information about the protocol of medical termination of pregnancy and were then admitted. Routine physical examination and investigations were carried out. Investigations included full blood count, urine routine examination, random blood sugar, blood group and rhesus factor, hepatitis screening, liver function tests, renal function tests and blood coagulation profile, quantitative HCG serum testing and STD were also performed.
Main outcome measures were the successful resolution of miscarriages without surgical intervention; secondary outcomes were the incidence of pain, vaginal bleeding, infection, pyrexia and gastrointestinal side effects.
After taking informed consent, misoprostol was inserted intravaginally in posterior fornix by a resident doctor in a dose of 800 mcg (4×200 mcg) with repeat dose every 3 to 4 h for total of 3 doses. Women who resided within Hyderabad city were allowed to go home with advice for follow up visit on third day, while others from rural areas were admitted. Women who did not completely expelled the products of conception on third day were administered a second dose of 800 mcg with advice for follow up on seventh day if the products of conception were still not completely expelled. The medical treatment was considered unsuccessful and a surgical evacuation was performed. Vital signs of vaginal bleeding and abdominal pain were assessed and adverse effects were recorded. Induction to expulsion interval was defined as the time in hours from initiation of therapy until the expulsion of products of conception. All data were collected in a predesigned proforma and were analyzed on SPSS version 16.0
RESULTS
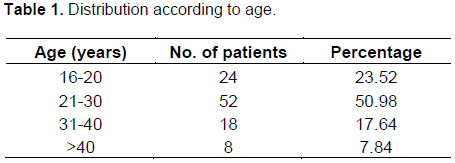
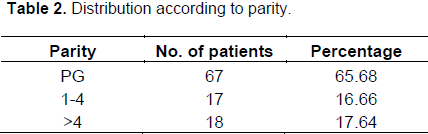
A total of 102 women were included in the study. Age range from 16 to 40 years and parity ranged from 0 to grand multipara (Table 1). Women were not selected according to parity but parity was a random occurrence. No relationship was found between parity and response to treatment with misoprostol (Table 2).
Incomplete abortion was found in 82 (80.39%), an embryonic pregnancy in 7 (6.86%) and early fetal demise in 13 (12.74%). Sixty four (62.74%) patients completely expelled the conceptual products on treatment with misoprostol alone, while 88 patients (37.25%) required surgical evacuation due to incomplete expulsion of conceptual products.
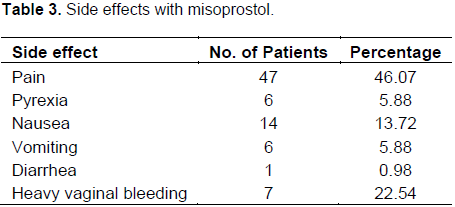
Mean induction to expulsion interval was 15.66 h. Main side effects noted were pain, pyrexia, nausea, vomiting and diarrhea. More than one side effect was noted in 7 (22.54%) patients (Table 3).
DISCUSSION
Termination of pregnancy for various reasons is a common obstetrical problem. Induction of abortion needs meticulous and effective care. The rate of maternal mortality and morbidity increases significantly by surgical methods for termination of pregnancy as compared to medical methods. Medical method has become a safe alternative to vacuum aspiration and dilatation and curettage (Blanchard et al., 2005; Borgatta et al., 2004; Creinin and Damry, 1993).
Misoprostol is the prostaglandin of choice as it is cheap and stable at room temperature. Different doses of oral or vaginal misoprostol have been used; however, the ideal dose and route is yet to be established (Khan et al., 2007). The regimen using repeated doses of misoprostol alone that can be finished within one day have the advantage of requiring less hospital visits and ultrasound examinations.
This study treatment with misoprostol resulted in complete expulsion of products of conception in 62.74% of the cases. In our study, successful abortion were found in 62.74% of the cases which is in accordance with other studies[14-17]. While a higher success rate of 80.4 and 90% was found in studies conducted by Borgattaet al. (2004), Jain et al. (2002, 2001).
Traditional methods of surgical evacuation of uterus are associated with major morbidity in up to 1% women and minor morbidity in 10%. Recently, misoprostol regimen has become more widely available and is now considered to be the gold standard for early pregnancy termination (Demetroulis et al., 2001; Faundes et al., 2007; Gemzell et al., 2007; Graziosi et al., 2004).
It was found that treatment with low dose regimens, that is, dose of 200 to 400 µg every 4 to 6 h were associated with less successful outcome as compared to our regimens of 800 mcg misoprostol. Szymarska et al. (2003) reported 30.0% success rate with the use of 400 µg of vaginal misoprostol and this success variation may be due to this reason. Differences in initial dosage, time interval during administrations, method and routes of drug administration, population and criteria for diagnosis of incomplete abortion were suggested to be relevant in explaining differences in outcome (Graziosi et al., 2004; Jain et al., 2002, 2001).
In our study, vaginal route was used for administration of misoprostol. Vaginal route appears to be the most effective, followed by sublingunal with oral being the least effective. Sublingunal misoprostol needs a more frequent administration, that is, every 3 h to achieve a similar effectiveness to the vaginal route (Kooper and Mishell, 1996; Kovavisarach and Jamnansiri, 2005; Mailre et al., 2000; Behrashi and Mahdian, 2009).
Incidence of pyrexia (5.88%), nausea (13.72%), vomiting (5.88%), diarrhea (0.98%), and heavy vaginal bleeding (22.54%), respectively. This is comparable to the study conducted by Mazhar et al. (2013). Oral and sublingual administration of misoprostol is associated with more gastrointestinal side effects than vaginal route. Abdominal pain was noted in 54.9% of women. It was much high in comparison to other studies (Wood and Brain, 2002; Neilsen et al., 1999). The incidence of heavy vaginal bleeding >500 ml was 22.54%. It was in contrast with the study conducted by Khan F.M when only 6.2% patient had heavy vaginal bleeding. None of the patient had pelvic inflammatory disease.
Age, parity and gestational age did not affect success route of medical abortion using misoprostol. Similar observation was noted in other studies (Neilsen et al., 1999; Zhang et al., 2005).
CONCLUSION
Treatment of early pregnancy loss with misoprostol is efficient, acceptable and cost effective for patients with complications of first trimester pregnancy loss.
CONFLICT OF INTEREST
None to declare
REFERENCES
Alberman E (1992). Spontaneous abortions: epidemiology. In: Stabile I, Grudzinskas G, Chard T, eds. Spontaneous abortion: diagnosis and treatment. London: Springer-Verlag 19-20. | |
| |
Awan AS, Bakhtiar U, Najeeb R (2008). Management of first trimester missed miscarriages with minimal surgical intervention. Pak Armed Forces Med. J. 58:437-44. | |
| |
Ballagh SA, Harris HA, Demasio K (1998). Is curettage needed for uncomplicated incomplete spontaneous abortion? Am. J. Obstet. Gynecol. 179:1279-82. | |
| |
Behrashi M, Mahdian M (2009). Comparison of medical (misoprostol) and surgical management for terminating first trimester abortion. Pak. J. Biological Sci. (9):1399-1401. | |
| |
Beucher G, Bellet T, Dryefus M (2003). Management of first trimester miscarriages. J Gynecol Obstetric Biol. Reprod. 32:5-21. | |
| |
Blanchard K, Shochet T, CoyajiK, Thi NN, Wini KB (2005). Misoprostol alone for early abortion: An evaluation of seven potential regimens. Contraception 72:91-97. | |
| |
Bogratee JS, Kullar V, Regan L, Moodely J, Kagoro H (2004). Randomized controlled trial comparing medical and expectant management of first trimester miscarriages. Hum. Reprod. 19:266-71. | |
| |
Borgatta L, Mullally B, Vragovic O, Gittinger E, Chen A (2004). Misoptrosol as the primacy agent for medical abortion in a low income urban setting. Contraception 70:121-16. | |
| |
Creinin MD, Damry PD (1993). Methotrexate and misoprostol for early abortion. Contraception 48: 339-48. | |
Demetroulis C, Saridogan E, Kunde D, Nafftalin AA (2001). A prospective randomized controlled trial comparing medical and surgical treatment for early pregnancy failure. Hum. Reprod. 16:365-69. | |
| |
Faundes A, Fiala C, Tang OS, Velasco A (2007). Misoprostol for the termination of pregnancy upto 12 completed weeks of pregnancy. Int. J. Gynecol. Obstet. 99:172-77. | |
| |
Gemzell DK, Ho PC, Gomez R, Weeks A, Winikoff B (2007). Misoprostol to treat missed abortion in the first trimester. Int. J. Gynaecol. Obstet. 99: 182-85. | |
| |
Graziosi GC, Mol BW, Ankum WH, Bruinse HW (2004). Management of early pregnancy loss. Int. J. Gynecol. Obstet. 86: 337-46. | |
| |
Jain JK, Dutton C, Hoeword B, Meckstroth KR, Mishell DR (2002). A prospective randomized double blinded placebo controlled trial comparing mifipristone and vaginal misoprostol to vaginal misoprostol alone for elective termination of early pregnancy failure. Hum. Reprod. 17:1477-82. | |
| |
Jain JK, Harwood B, Meckstoth KR, Mishell DR (2001). Early pregnancy termination with vaginal misoprotol combined with Loperamide and acetaminophen. Contraception 63:217-21. | |
| |
Jurkovic D, Ross JA, Nicolaides KH (1998). Expectant management of missed miscarriage. Br. J. Obstet. Gynaecol. 105:670- 1. | |
| |
Khan FM, Amin A, Ahmed FI, Naeem NK (2007). Medical Termination of Frist Trimester Miscarriages. Annals 13(2):154-157. | |
| |
Kooper TB, Mishell DR (1996). The use of misoprostol for termination of early pregnancy. Contraception 53:237-42. | |
| |
Kovavisarach E, Jamnansiri CH (2005). Intravaginal misoprostol 600 and 800ug for the treatment of early pregnancy failure. lnt. J. Gynecol. Obstet. 90:208-12. | |
| |
Luise C, Jermy K, May C, Costello G, Collins WP, Bourne TH (2002). Outcome of expectant management of spontaneous first trimester miscarriage: observational study BMJ 324:873-5. | |
| |
Macrow P, Elstein M (1993). Managing miscarriage medically. BMJ 306:876. | |
| |
Mailre SC, Bouchard P, Spitz M (2000). Medical termination of pregnancy. N. Eng. J. Med. 342:946-56. | |
| |
Mazhar T, Naveed P, Fatima S (2013). Management of first trimester missed abortions with misoprostol. J. Med. Sci. 21(3):114-117. | |
Neilsen S, Hahlin M, Jens PC (1999). Randomized trial comparing expectant with medical management for first trimester miscarriages. Br. J. Obstet. Gyneacol. 106:804-807. | |
Wood SL, Brain PH (2002). Medical management of missed abortion: A randomized clinical trial. Obstet. Gynecol. 99:563-66. | |
Zhang J, Gilfes JM, Barnhant K, Creinin MD, Westhoff C, Frederick MM (2005). A comparison of medical management with misoprostol and surgical management for early pregnancy failure, N. Engl. J. Med. 353:761-69. | |