Reasons for admission and mortalities following admissions in the intensive care unit of a specialized hospital, in Ethiopia


Published: Sept. 30, 2014
Latest article update: Aug. 19, 2022
Abstract
Many studies have been conducted in the intensive care unit (ICU). But little is known about the outcomes of ICU admissions. This is particularly the case in the ICU of developing countries. Thus, the aim of this study was to assess reasons and outcomes of admissions in the ICU of Jimma University Specialized Hospital (JUSH). A longitudinal study was conducted in the ICU of JUSH from February 7 to April 15, 2011. All patients admitted to the ICU during the study period were followed till discharge or death. Data was coded and entered into the Statistical Package for Social Sciences (SPSS) windows version 16.0 to generate descriptive statistics. Sixty nine patients admitted to the ICU during the study period were followed prospectively till discharge or death. Diseases of cardiovascular origin (30.4%) followed by surgical interventions (18.8%) were the major reasons of ICU admission. There were 26 (37.7%) deaths during the study period in the ICU. Mortality rate in the ICU was found to be significantly high. Diseases of cardiovascular origin were the major reasons for ICU admission. Hence, responsible bodies need to seek for possible ways of reducing this unacceptably high mortality in the ICU by devising quality control mechanisms.
Keywords
Intensive care unit., outcome of admission, Reasons of admission
INTRODUCTION
Hospitalization should occur or should be considered depending on each patient’s presenting symptoms and physical examination. The decision to admit patients to the medical wards was determined by age, co-existing illness, physical and laboratory findings, the ability of the patient to comply reliably with an oral medication, and the resources available to the patient outside the hospital (Dipiro et al., 2008; Mandell and Wunderink, 2008). The death rate in the medical wards of Jimma University Specialized Hospital (JUSH) was reported to be 12.6%, communicable diseases being the most common reasons for admission (Ali and Woldie, 2010).
Most patients do not require admission to the intensive care unit (ICU) and are admitted to a monitored unit or general medical floor. ICU is a consolidated area of a hospital where patients with acutely life threatening illnesses or injuries receive around the clock specialized medical and nursing care, such as mechanical ventilation and intensive cardiac monitoring (Kohn et al., 2000; Leapfrog Group, 2014). Admission to an ICU may be required if the patient experiences hemodynamic instability requiring frequent monitoring of vital signs, invasive hemodynamic monitoring, or rapid titration of intravenous medications with concurrent monitoring to assure safe and effective outcomes (Dipiro et al., 2008; Mandell and Wunderink, 2008). Apart from causing death, the type and severity of illnesses can directly affect the length of stay in the ICU. Although ICU admis-sion for asthma is relatively uncommon, it remains to be associated with appreciable in-hospital mortality (Lange et al., 2009; Mayr et al., 2006; Gruenberg et al., 2006; Roch et al., 2011; Gupta et al., 2010).
Planned surgery (43%), infection (12.1%), sepsis (10.1%) and cardiac arrest (8.0%) were the most common reasons for ICU admission among which 10.9% of the patients died while they are in the ICU. Similar mortality rate was reported from another ICU, 9.5% (Lange et al., 2009; Mayr et al., 2006). On the other hand, mortality rate as high as 26% has also been reported by one study (Enget al., 1992).
The estimated mean in France, in a multi-center study, is about 15% for ICU mortality and 6 to 25% for hospital mortality after ICU discharge, yielding a hospital mortality rate of 20 to 30%, with substantial variations across studies (Azoulay et al., 2003). A recent systematic review revealed that patients admitted to an ICU over the weekend appear to be at an increased risk of death, while nighttime admissions were not associated with an increased mortality (Cavallazzi et al., 2010). On the other hand, a study reported from Canada concluded that time of admission does not have significant effect on outcome of patients admitted to the ICU (Ala et al., 2011). A study on acute myeloid leukemia showed that survival was inferior in those patients admitted to the ICU compared to those who were not admitted. However, no difference between intensive care and non-intensive care patients was found concerning continuous complete remission at 6 years or survival at 6 years (Schellongowski et al., 2011).
However, much cannot be said about ICUs in Ethiopia since there are no studies so far. Therefore, this study is reporting the findings of the analysis done from the data collected primarily to pick medication errors at the ICU of JUSH (Agalu et al., 2011). This analysis aimed to identify reasons for admission and outcomes of admissions to the ICU in JUSH.
METHODOLOGY
Study area and design
The longitudinal study was conducted as part of broader cross-sectional study on medication errors (Agalu et al., 2011, 2012) from February 7 to April 15, 2011 in the ICU of Jimma University Specialized Hospital (JUSH), a teaching hospital located in Jimma town, Southwestern Ethiopia, 350 km from Addis Ababa. JUSH is the only referral hospital in Southwest Ethiopia with 450 beds and 558 health professionals where a multidisciplinary team of diverse professionals provide a range of health care services for approximately 9000 inpatients and 80,000 outpatients each year. The ICU has 6 beds serving patients from the different departments of the hospital (Jimma University Specialized Hospital, 2014).
Participants
All critically ill patients who were admitted to the ICU of JUSH during the study period were included in the study. All patients admitted to the ICU during the study period were followed till discharge or death. Patient cards and medication documentation charts were also reviewed.
Data collection and management
Data was collected using a pre-tested structured data collection format by one trained clinical pharmacy post-graduate student together with principal investigator. Since this paper is the product of the broader study on, accessory data was compiled from that study. The content of the format included demographic variables, diagnoses and co-morbidities, dates and time of prescription, name of the medication, dosage forms, doses, frequency, and duration of medications prescribed. Demographic information about patients was obtained from patient card and medication charts. Diagnosis made by physicians was taken from patient cards. Finally, the data was edited, coded, entered into SPSS windows version 16.0 and finally cleared. Descriptive statistics were generated to meet the objective.
Ethical considerations
Prior to the study, ethical approval was obtained from the Ethical Review Board of Jimma University. The management of the hospital was requested for cooperation with formal letter. Written consent was obtained from the nurses, physicians and patients included in the study and names of patients and the health professionals were replaced with their initials. All data obtained in the course of the study were kept confidentially and used solely for the purpose of the study.
RESULTS
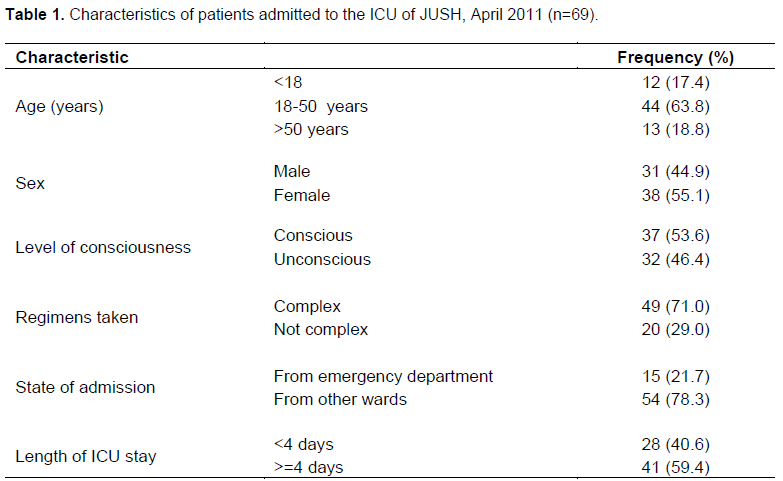
About 69 patients were admitted to the ICU during the data collection period (9 weeks period). Majority of these patients were females 38 (55.1%) and in the age group of 18 to 50 years, 44 (63.8%) (Mean age of 32.87 ± 17.03 years). About 54 (78.3%) of them were admitted to other wards before they come to the ICU, about 32 (46.4%) were unconscious and 49 (71.00%) received complex regimen (average of 5 ± 2 drugs). Patients stayed 5.654 ± 5.22 days in the ICU till death/transfer to other wards. Average number of co-morbid conditions per patient was 3 ± 2. (Table 1).
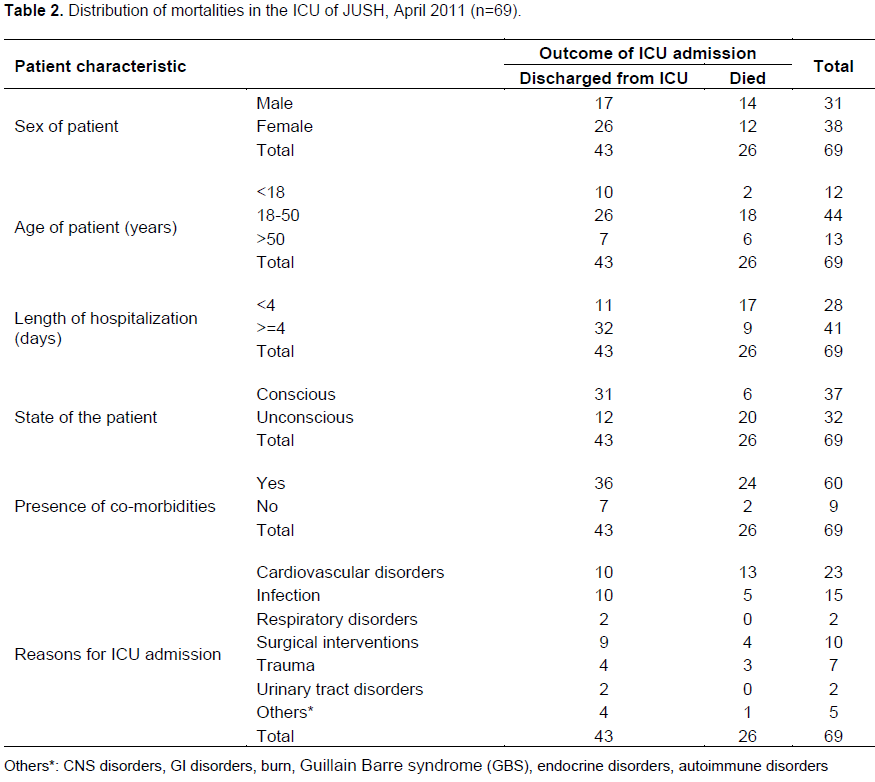
Twenty six (37.7%) patients died during the 9 weeks period. Eighteen (69.2%) patients who died in the ICU were in the age group of 18-50 years while 14 (53.8%) of the patients who died in the ICU were males. Nineteen (73.1%) of the patients who died in the ICU were admitted in other wards prior to ICU admission while 7 (26.9%) of the deaths were among patients directly admitted to the ICU from the emergency department (Table 2).
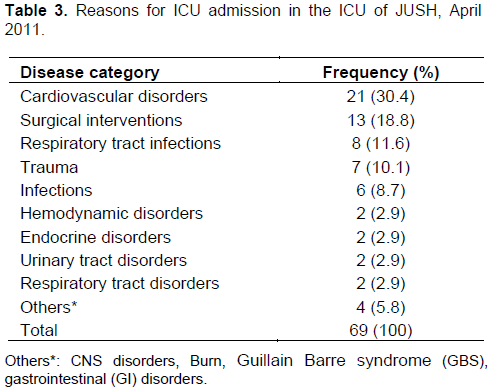
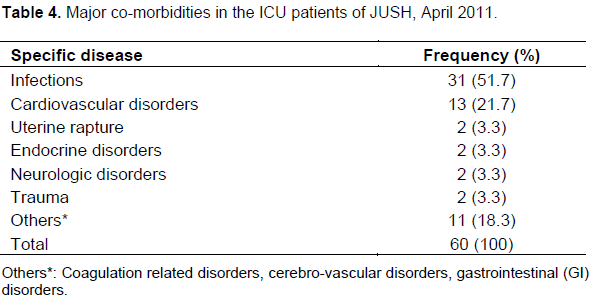
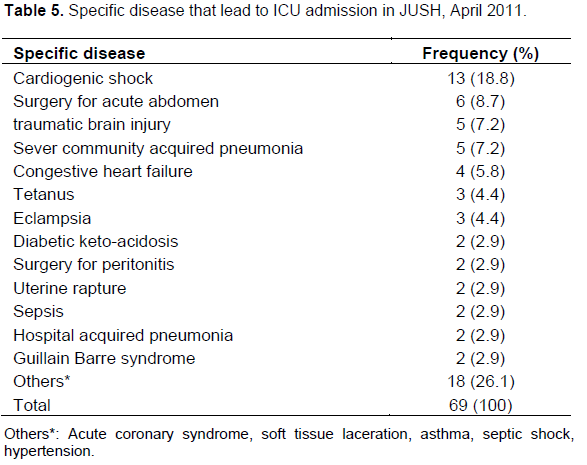
Common diagnoses that lead to ICU admission were diseases of cardiovascular origin 21 (30.4%), followed by surgical interventions for various reasons 13 (18.8%) and respiratory tract infections 8 (11.6%) (Table 3). Infectious diseases were the commonest (51.7%) co-morbid conditions in patients admitted to the ICU followed by cardiovascular disorders (21.7%) (Table 4). On the other hand, cardiogenic shock (18.8%), surgical interventions (8.7%), traumatic brain injury (7.2%) and sever community acquired pneumonia (7.2%) were common specific diseases that led to ICU admission (Table 5).
DISCUSSION
According to this study, the commonest diagnoses that lead to ICU admission were diseases of the cardiovascular system (30.4%) followed by surgical interventions of various reasons (18.8%) and respiratory tract infections (11.6%). Similar finding was reported from Austria (Lange et al., 2009) but it was different from what was found in the medical wards of JUSH (Ali and Woldie, 2010), where infectious diseases were the commonest causes of admission.
In this study, infectious diseases were the commonest (51.7%) co-morbid conditions followed by cardiovascular disorders (21.7%). This is similar with the finding in the medical wards of JUSH. This might be explained by the fact that majority of the ICU admissions in the JUSH come from the medical wards where patients with chronic diseases often have co-morbid infectious (Ali and Woldie, 2010). Unlike the previous study where severe community acquired pneumonia, pyogenic and chronic meningitis, and malaria were common (Ali and Woldie, 2010), the present study showed that cardiogenic shock, surgical interventions and traumatic brain injury were the major reasons that lead to ICU admission. This difference might me due to the difference in the ward where ICU only serves severe cases as compared to the general medical wards.
The death rate in the ICU was 26 (37.7%) which was higher than findings reported in earlier works from France (multi-center study), ICU of Asthma in London and JUSH (Ali and Woldie, 2010; Gupta et al., 2004; Azoulay et al., 2003). On the other hand, it is lower than the finding of a study from Australia (Lange et al., 2009). The differences observed in this regard might be related to the difference in patient profile and the ICU setting in which the patients were managed. Being the part of broader study in medication errors and based on accessory data, this study did not assessthe severity of disease conditions during admission.
Similarly, it did not calculate prognostic score, standard mortality ratio, comorbidity index and did not use Glasgow Coma Scale to determine the level of consciousness. It has to be noted that this study did not consider death of patients after discharge from the ICU. Moreover, it did not determine all the possible causes for death including medication errors. Since patient cards and medication charts were reviewed prospectively, all the diseases and co-morbidities patients had not been identified during data collection.
All these might affect the quality of data, thus should be used as the possible insights for the future studies in the ICU.
In conclusion, diseases of cardiovascular origin were the major reasons for ICU admission and there were significant deaths among admissions in the ICU. Hence, responsible physicians and others concerned need to seek for possible ways of reducing this unacceptably high mortality in the ICU by determining the causes for it. Supporting such efforts with further studies to identify predictors of mortality in the ICU is warranted.
COMPETING INTERESTS
The authors declare that they have no competing interests.
ACKNOWLEDGEMENT
The authors are thankful for the funding they received from Jimma University during the conduct of this study.
REFERENCES
Ala S, Pakravan N, Ahmadi M (2011). Mortality Rate and Outcome among Patients Admitted to General Intensive Care Unit during "Morning-Hour" Compared with" Off-Hour". Canadian J. Med. 2(5).Accessed on 29/12/2011 at: http://ampublisher.com/Dec%202011/CJM-1112-015-Mortality-Rate-Outcome-Patients-Admitted-General-Intensive-Care.pdf | |
| |
Ali E, Woldie M (2010). Reasons and Outcomes of admissions to the medical wards of Jimma University Specialized Hospital, Southwest Ethiopia. Ethiop. J Health Sci. 21(2):113-120 | |
| |
Azoulay E, Adrie C, De Lassence A, Pochard F, Moreau D, Thiery G, Cheval C, Moine P, Garrouste-Orgeas M, Alberti C, Cohen Y, Timsit JF (2003). Determinants of post intensive care unit mortality: a prospective multicenter study. Crit. Care Med. 31:428-432. | |
| |
Cavallazzi R, Marik PE, Hirani A, Pachinburavan M, Vasu TS, Leiby BE (2010). Association between Time of Admission to the ICU and Mortality: A Systematic Review and Meta analysis. Chest 138(1):68-75. | |
| |
Dipiro J, Talbert B, Yee GC, Matzke GR, Wells BG, Posey LM (2008). Pharmacotherapy: A Pathophysiologic Approach,7th edition. McGraw-Hill, Medical Publishing Division | |
| |
Eng PCT, Chng HH, Feng PH (1992). Mortality patterns in a medical intensive care unit. Singapore Med. J. 33:24-26. | |
| |
Friesenecker BE, Takala J, Hasibeder WR (2006). Causes of death and determinants of outcome in critically ill patients. Crit. Care 10(6):1-13 | |
| |
Gruenberg DA, Shelton W, Rose SL, Rutter AE, Socaris S, McGee G (2006). Factors Influencing Length of Stay in the Intensive Care Unit. Am. J. Crit. Care 15:502-509. | |
| |
Gupta D, Keogh B, Chung KF, Ayres JG, Harrison DA, Goldfrad C, Brady AR, Rowan K (2004). Characteristics and outcome for admissions to adult, general critical care units with acute severe asthma: a secondary analysis of the ICNARC Case Mix Program Database. Critical Care 8(2):1-10. | |
| |
Kohn LT, Corrigan JM, Donaldson MS (2000). To err is human: Building a safer health system. Washington, DC: National Academy Press. IOM document repository. Vol. 627. Accessed 15/11/ 2010 | |
| |
Lange DW, Dusseljee J, Brinkman S, Berkel G, van Maanen R, Bosma RJ (2009). Severity of illness and outcome in ICU patients in the Netherlands: results from the NICE registry 2006-2007. Neth J. Crit. | |
| |
Leapfrog Group (2014), ICU physician staffing. Fact sheet. The Leapfrog group for patient safety rewarding higher standards. Accessed 15/11/ 2010. | |
| |
Mandell LA, Wunderink R (2008). Community Acquired Pneumonia: Treatment, Site of Care. In: Kasper LD, Braunwald E, Fauci AS, Hauser LS, Longo LD, Jameson JL, editors. Harrison's Principles of Internal Medicine. 17th ed. New York: McGraw-Hill 1622-1623. | |
| |
Mayr VD, Dünser MW, Greil V, Jochberger S, Luckner G, Ulmer H, Roch A, Wiramus S, Pauly V, Forel JM, Guervilly C, Gainnier M, Papazian L (2011). Long-term outcome in medical patients aged 80 or over following admission to an intensive care unit. Crit. Care 15(36):1-7 | |
| |
Schellongowski P, Staudinger T, Kundi M (2011). Prognostic factors for intensive care unit admission, intensive care outcome, and post-intensive care survival in patients with de novo acute myeloid leukemia: a single center experience. Haematologica 96(2). | |